The Dangerous Connection: Diabetes, Neuropathy, and Foot Ulcers
Diabetes is a chronic condition affecting millions worldwide, but its impact extends far beyond blood sugar management. One of the most serious and debilitating complications is the development of foot ulcers, which can lead to severe infections and even amputation. Understanding the dangerous connection between diabetes, nerve damage (neuropathy), and poor circulation is the first step toward prevention.
The Cascading Effect: From High Blood Sugar to Serious Risk
The journey from a well-managed condition to a life-altering foot problem follows a predictable, yet preventable, path. This progression is often described as a triad of complications: neuropathy, vascular insufficiency, and trauma.
1. High Blood Sugar (Hyperglycemia): The starting point is persistently high blood glucose levels. Over time, this excess sugar damages various body systems, most notably the nerves and blood vessels. According to the Mayo Clinic, high blood sugar injures nerve fibers throughout the body, with nerves in the legs and feet being the most commonly affected.
2. Diabetic Neuropathy: This nerve damage leads to a loss of "protective sensation." You may no longer feel pain, heat, or cold in your feet. As the Centers for Disease Control and Prevention (CDC) explains, pain is the body's alarm system. Without it, a small cut, blister, or sore can go completely unnoticed.
3. Unnoticed Injury: Because of the numbness, everyday occurrences like a pebble in a shoe or a poorly fitting pair of shoes can cause skin breakdown without the person realizing it.
4. Foot Ulcer Formation: The unnoticed injury can quickly develop into an open sore, known as a diabetic foot ulcer (DFU). These are typically full-thickness wounds that penetrate the dermis.
5. Infection and Amputation: Compounded by poor blood flow (peripheral artery disease), which also results from diabetes, these ulcers struggle to heal. They become highly susceptible to infection, which can spread to the underlying tissue and bone. If the infection cannot be controlled, amputation may be necessary to prevent it from spreading further and to save the patient's life.
Understanding the Core Problems
To effectively prevent foot ulcers, it's crucial to understand the underlying mechanisms that create the "perfect storm" for their development.
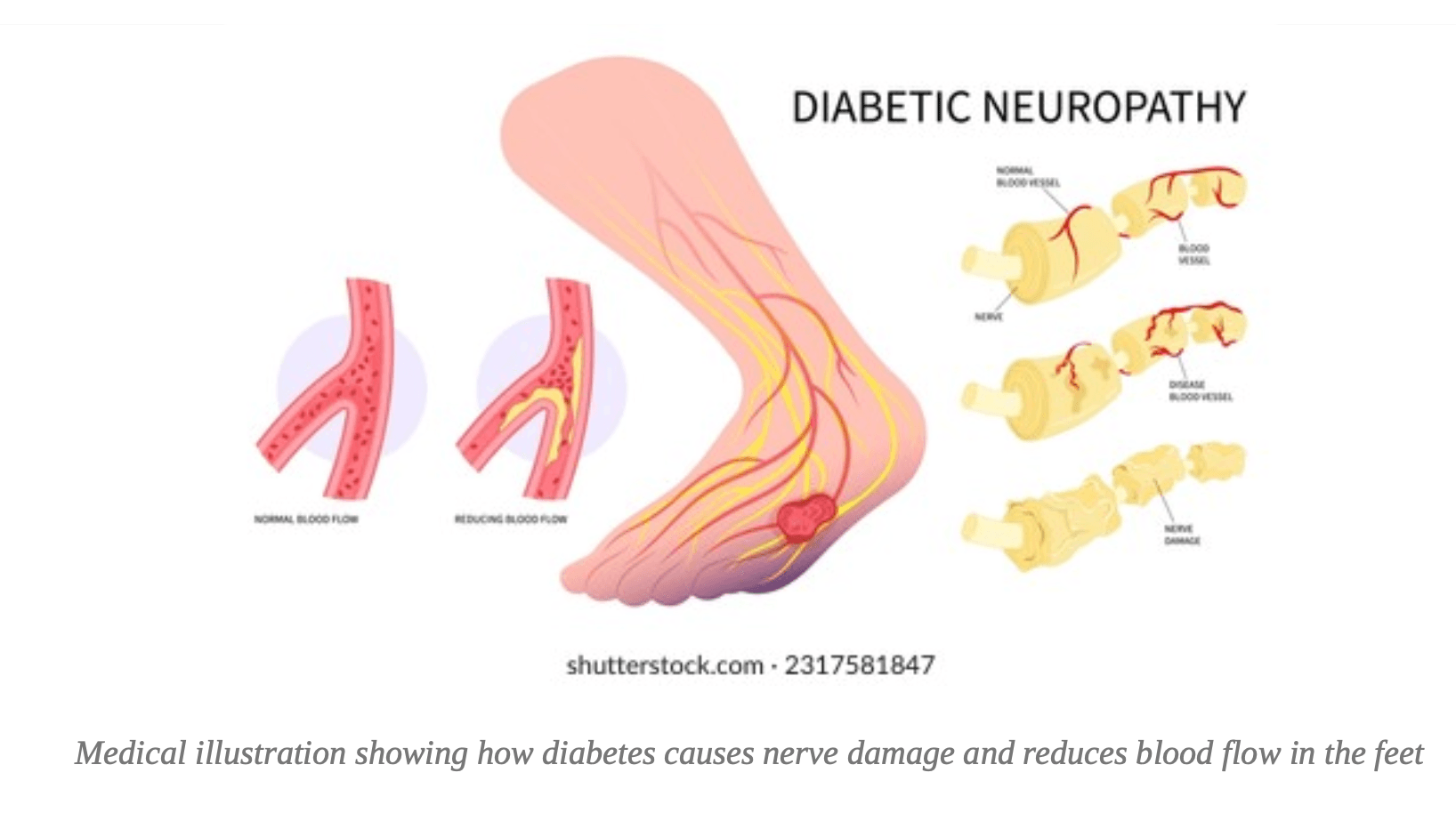
Diabetic Neuropathy: The Silent Threat
Diabetic neuropathy is not a single condition but a family of nerve disorders caused by diabetes. It is the leading cause of diabetic foot ulcers. The CDC reports that about half of all people with diabetes have some form of nerve damage. Neuropathy manifests in several ways in the feet:
Sensory Neuropathy: This is the loss of sensation, which eliminates the warning signs of injury. Patients may experience tingling or burning pain initially, which can progress to complete numbness.
Motor Neuropathy: Damage to the nerves that control foot muscles leads to an imbalance, causing foot deformities like hammertoes and bunions. These deformities create abnormal pressure points that are prone to ulceration. Research published in PMC highlights this as a direct cause of skin breakdown.
Autonomic Neuropathy: This affects the body's involuntary functions, including sweat production. Reduced sweating leads to dry, cracked skin, which provides an easy entry point for bacteria.
Peripheral Artery Disease (The Healing Barrier)
Peripheral Artery Disease (PAD) is another common complication of diabetes, present in up to 50% of patients with foot ulcers. Diabetes promotes atherosclerosis, a condition where plaque builds up and narrows the arteries. This significantly reduces blood flow to the lower extremities.
Poor circulation creates two major problems:
1. It deprives the tissues of the oxygen and nutrients needed for wound healing.
2. It hinders the body's ability to fight infection by limiting the transport of immune cells to the wound site.
This is why a small, seemingly minor wound on a diabetic foot can fail to heal and become a chronic, infected ulcer.
Foot Ulcers: When Small Wounds Become Major Threats
A diabetic foot ulcer is an open sore or wound that occurs in approximately 15% of patients with diabetes. They are most common on the bottom of the foot or over pressure points. Without the ability to feel the initial injury and with compromised healing due to poor blood flow, these ulcers can deepen, exposing ligaments, tendons, and even bone. Data shows that 80% of lower-limb amputations in people with diabetes are preceded by a foot ulcer, underscoring the critical need for prevention and early intervention.
Prevention is Key: Protecting Your Feet
The good news is that most serious foot complications can be prevented. A combination of diligent self- care and regular professional oversight is the most effective strategy.
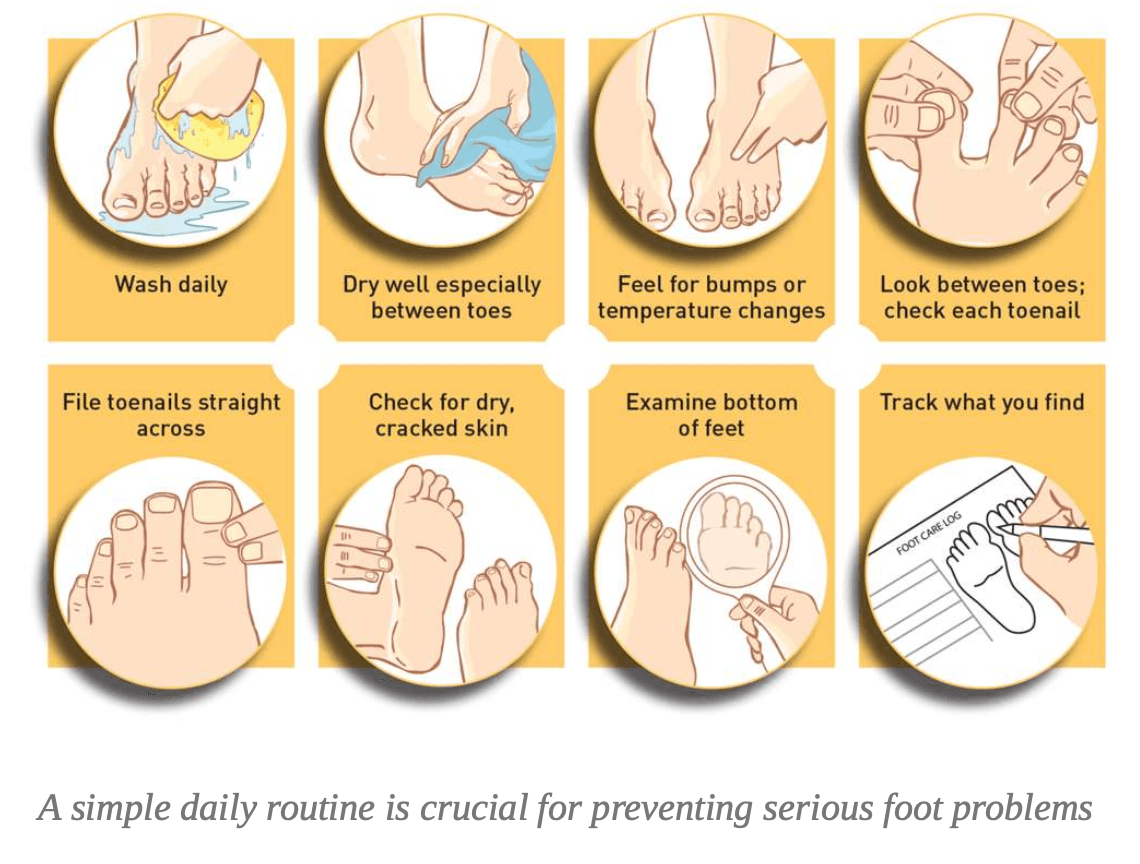
Daily Foot Care: Your First Line of Defense
Integrating a simple foot care routine into your daily life can make all the difference. The CDC recommends the following steps:
Check your feet every day. Look for cuts, sores, blisters, redness, calluses, or any other changes. Use a mirror or ask a family member for help if you can't see the bottoms of your feet.
Wash your feet every day. Use warm (not hot) water and mild soap. Dry them thoroughly, especially between the toes.
Keep skin soft and smooth. Apply a thin coat of lotion over the tops and bottoms of your feet, but not between your toes, to prevent moisture buildup that can lead to infection.
Never go barefoot. Always wear shoes and socks, even indoors, to protect your feet from injury. Wear shoes that fit well. Choose comfortable shoes with ample toe room. Always check inside your shoes for foreign objects before putting them on.
Trim your toenails straight across. Gently file any sharp edges. If you have trouble, have a podiatrist (foot doctor) do it for you.
Don't remove corns or calluses yourself. This can lead to injury and infection. Seek professional care.
Professional Medical Care: Your Essential Partner
Self-care is vital, but it must be paired with regular medical attention. A multidisciplinary approach involving your primary care physician, endocrinologist, and a podiatrist is recommended.
"Podiatrists play a key role in detecting and treating foot problems in people with diabetes. These include neuropathy (nerve damage), arthropathy (joint damage), and vasculopathy (blood vessel damage). Complications can be avoided or delayed with yearly comprehensive foot exams and treatment." - CDC Guidance for Clinicians
Be sure to:
Get a comprehensive foot exam at least once a year. This exam should assess sensation, blood flow, and foot structure.
Have your feet checked at every healthcare visit. Take off your socks and shoes so your doctor can quickly inspect them.
See your doctor immediately if you notice any of the following: pain or cramping in your legs, tingling or burning, a change in foot shape or color, or any blister, sore, or ulcer.
Debunking Common Myths About Diabetic Foot Care
Misinformation can be just as dangerous as neglect. Here are some common myths and the facts you need to know:
Myth: "If my feet don't hurt, they are healthy."
Fact: This is one of the most dangerous misconceptions. Neuropathy's primary symptom is a lack of pain. You could have a serious injury and not feel it at all. Daily visual inspection is non- negotiable.
Myth: "Soaking my feet in a hot bath is a good way to clean them."
Fact: Soaking can dry out the skin, making it more prone to cracking. Furthermore, if you have an open wound, soaking can expose it to bacteria. It's better to wash your feet in the shower and dry them thoroughly.
Myth: "It's okay to use alcohol or hydrogen peroxide to clean a small cut."
Fact: These substances are too harsh and can damage healthy skin cells, which slows down the healing process. Mild soap and water are the best choice for cleaning a minor wound.
Conclusion: Take Control to Save Your Feet
The link between diabetes, neuropathy, and foot ulcers is a serious threat, but it is not an inevitability. By understanding the risks and taking proactive steps, you can significantly reduce your chances of developing severe complications. The cornerstones of prevention are:
1. Managing your diabetes: Keeping your blood sugar, blood pressure, and cholesterol levels within your target range is the most important thing you can do to prevent or delay complications.
2. Practicing diligent daily foot care: A few minutes each day can save you from months of difficult treatment.
3. Engaging with your healthcare team: Regular professional check-ups can catch problems early when they are most treatable.
Take control of your foot health today. Understanding the connection is the first step, but consistent action is what will ultimately save lives and feet.
Reference
[1] Foot Care | Diabetes Standards of Care and Resources for ...
https://www.ihs.gov/diabetes/clinician-resources/soc/foot-care1/
[2] Understanding diabetic foot - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC2878694/
[3] Mechanisms of diabetic foot ulceration: A review - PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC10101842/
[4] Tips for Healthy Feet Graphic | Diabetes
https://www.cdc.gov/diabetes/communication-resources/tips-for-healthy-feet.html
[5] [PDF] Foot Health | Healogics
https://www.healogics.com/wp-content/uploads/2021/03/Healogics-Foot-Health-Infographic-2021.p df
[6] Your Feet and Diabetes
https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-your-feet.html
[7] Promoting Foot Health | Diabetes
https://www.cdc.gov/diabetes/hcp/clinical-guidance/diabetes-podiatrist-health.html
[8] Diabetic neuropathy - Symptoms & causes - Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-2037158 0
